The mathematical approach that could change coronavirus tests

Scientists say that popular testing is wanted to get outbreaks of the new coronavirus less than handle. But in several locations there’s a shortage of the chemicals desired to run exams. In quite a few countries, overall health officers have started out making use of a tactic that was initial proposed in the Second Globe War: team screening. By tests samples from quite a few folks at when, this method can help you save time, chemical reagents and dollars, say researchers.
“In the latest epidemic, there is a want to exam an extremely big range of people, making pooling an interesting alternative,” says Roy Kishony, a methods biologist at Technion — Israel Institute of Technology in Haifa.
China, India, Germany and the United States are currently using team testing.
There are numerous ways to conduct group screening, and experts in a number of nations around the world are experimenting with the very best technique for executing this through a pandemic. Their thoughts largely arrive from a field of arithmetic recognized as group screening, which has been broadly used — from detecting defective Xmas-tree lights to estimating the prevalence of HIV in a populace. “There has been a flurry of innovation in this subject,” says Dror Baron, an details scientist at North Carolina Condition College in Raleigh.
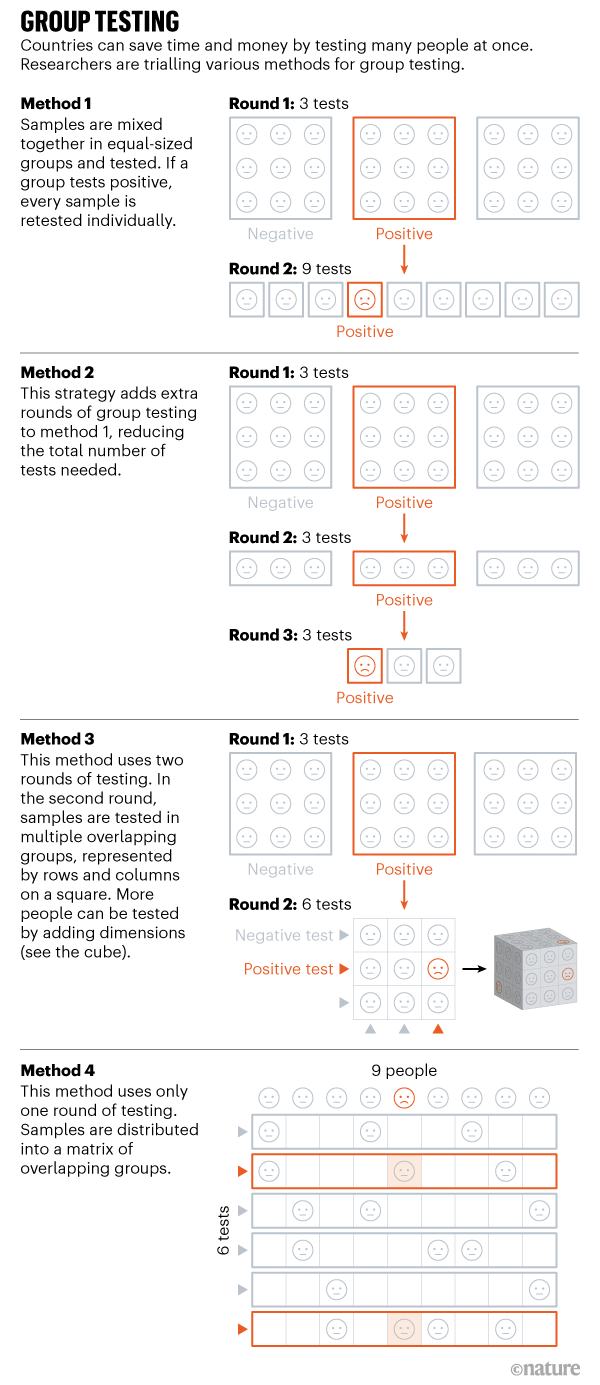
Nature highlights four solutions currently being trialled.
System 1 & 2: From syphilis to coronavirus
The most easy technique for team tests was proposed by economist Robert Dorfman in the 1940s to take a look at troopers for syphilis.
In this method, an equal range of samples — gathered from nasal and throat swabs in the scenario of the SARS-CoV-2 coronavirus — are blended together (see Technique 1) and analyzed at the time. Teams of samples that take a look at negative are dominated out. But if a group checks good, every single sample in that team is then retested individually. Scientists estimate the most effective group sizing — the 1 that utilizes the minimum quantity of checks — on the foundation of the prevalence of the virus in the neighborhood.
In May perhaps, officials in Wuhan, China, made use of this strategy as aspect of their initiatives to test the large bulk of the city’s population, reaching approximately ten million folks in just about two weeks. Samples from some 2.3 million individuals had been team analyzed, with up to 5 samples in a team, and 56 infected people were being determined.
The system is most effective when there are low concentrations of infection, in around 1% of the populace, simply because team checks are a lot more most likely to be detrimental, which will save tests numerous individuals individually, say scientists.
“This is likely the easiest process,” says Krishna Narayanan, an information theorist at Texas A&M University in University Station. But there are additional productive strategies to build the next stage than testing every person individually, he says.
A extra sophisticated edition consists of introducing extra rounds of team exams, ahead of tests just about every sample independently (see Process 2). Incorporating rounds reduces the variety of men and women who need to be analyzed independently.
But this solution is sluggish, mainly because it usually takes many several hours to get the effects for every group check, suggests Wilfred Ndifon, a theoretical biologist at the African Institute for Mathematical Sciences in Kigali, Rwanda. “This is a rapidly-increasing, rapidly-spreading condition. We need to have solutions significantly quicker than this solution would permit,” he suggests.
Technique 3: Multi-proportions
Ndifon and his colleagues have improved on Dorfman’s system, which they system to demo in Rwanda, and so in the end reduce the amount of exams needed. Their initial spherical of team exams is the exact same as Dorfman’s, but for teams that exam optimistic, they suggest a second spherical that divides samples among the teams that overlap.
Consider a sq. matrix with nine models, each and every symbolizing swabs taken from a single particular person (see Process 3). The samples in every row are tested as just one team, and the samples in each and every column are analyzed as one particular team, ensuing in 6 checks in full, with each and every person’s sample remaining in two groups. If a sample incorporates SARS-CoV-2 viral RNA, each of the team exams will be good, earning it simple to discover the person. Researchers explain the concept in a preprint posted on the arXiv server on 30 April1.
Raising the amount of proportions, for example from a square to a dice, lets for larger sized team dimensions and larger gains in effectiveness, claims Neil Turok, a theoretical physicist at the College of Edinburgh, United kingdom, and is a review co-writer.
Ndifon, who is aspect of Rwanda’s COVID-19 endeavor pressure, suggests group screening is section of the government’s tactic to speedily recognize and isolate infected men and women. He and his colleagues estimate that their strategy could lower the price of testing from US$9 per person to 75 cents. The researchers are carrying out laboratory experiments to see how numerous samples can basically be included in a team check and nonetheless detect a constructive end result. Leon Mutesa, a geneticist at the University of Rwanda in Kigali, and one more co-writer who is element of the govt endeavor power, says that he has been in a position to discover 1 beneficial sample in a pool of 100 in the lab.
But Sigrun Smola, a molecular virologist at Saarland College Healthcare Middle in Homburg, Germany, who has been screening samples in teams of up to 20, doesn’t recommend grouping more than 30 samples in one check, to guarantee adequate accuracy. Larger groups will make it tougher to detect the virus, and increase the likelihood of missing positives, she suggests. Smola is also sceptical of the functional application of the dice-slicing system in program screening. “If you advised this to a technician, they would say ‘What a mess. I want a uncomplicated scheme’,” she adds.
Ndifon says that his workforce plans to acquire application to automate the placement of samples.
Process 4: One particular-phase remedy
Some researchers say that even two rounds of testing is as well many when striving to control a fast-spreading virus this kind of as SARS-CoV-2. Lab experts need to wait around for the success from the 1st round to come via, which slows the system, suggests Manoj Gopalkrishnan, a laptop scientist at the Indian Institute of Know-how Bombay.
As an alternative, Gopalkrishnan proposes carrying out all the exams in a person round, with numerous overlapping teams. This would enhance the range of exams, but would conserve time — despite the fact that the first established-up is time consuming, since acquiring further groups signifies extra samples need to be pipetted.
Gopalkrishnan’s solution requires mixing samples in distinct teams, making use of a counting system identified as Kirkman triples, which sets rules for how the samples should really be distributed. Picture a flat matrix in which each row signifies a single check, and just about every column signifies 1 man or woman (see Technique 4). Typically, every single examination ought to contain the exact same selection of samples, and just about every person’s sample must be analyzed the exact same variety of moments.
But Narayanan suggests that 1-stage techniques call for far more assessments to make certain the exact same degree of precision as for multi-phase group tests. A single-step strategies also signify doing the job with a substantial variety of samples at once, which can be difficult, he says. “It is not possible for a technician to do this pooling. You would need a robotic technique.”
To simplify the course of action in the lab, Gopalkrishnan and his colleagues have formulated a smartphone application that tells customers how to mix the samples. In unpublished outcomes from clinical trials in India in Mumbai, Bangalore and Thalassery, he suggests, 5 good samples were being properly determined out of 320 working with only 48 exams.
Researchers in Israel are working with an automated process and an application to use a identical a single-stage process. Moran Szwarcwort-Cohen, who heads the virology lab at Rambam Wellness Treatment Campus in Haifa, says her group is presently evaluating the method, with promising success.

Twitter fan. Beer specialist. Entrepreneur. General pop culture nerd. Music trailblazer. Problem solver. Bacon evangelist. Foodaholic.